Opioid-Related DDI Involving Short-Term Antimicrobial
This is an example scenario based on real medication compliance results.
Challenge
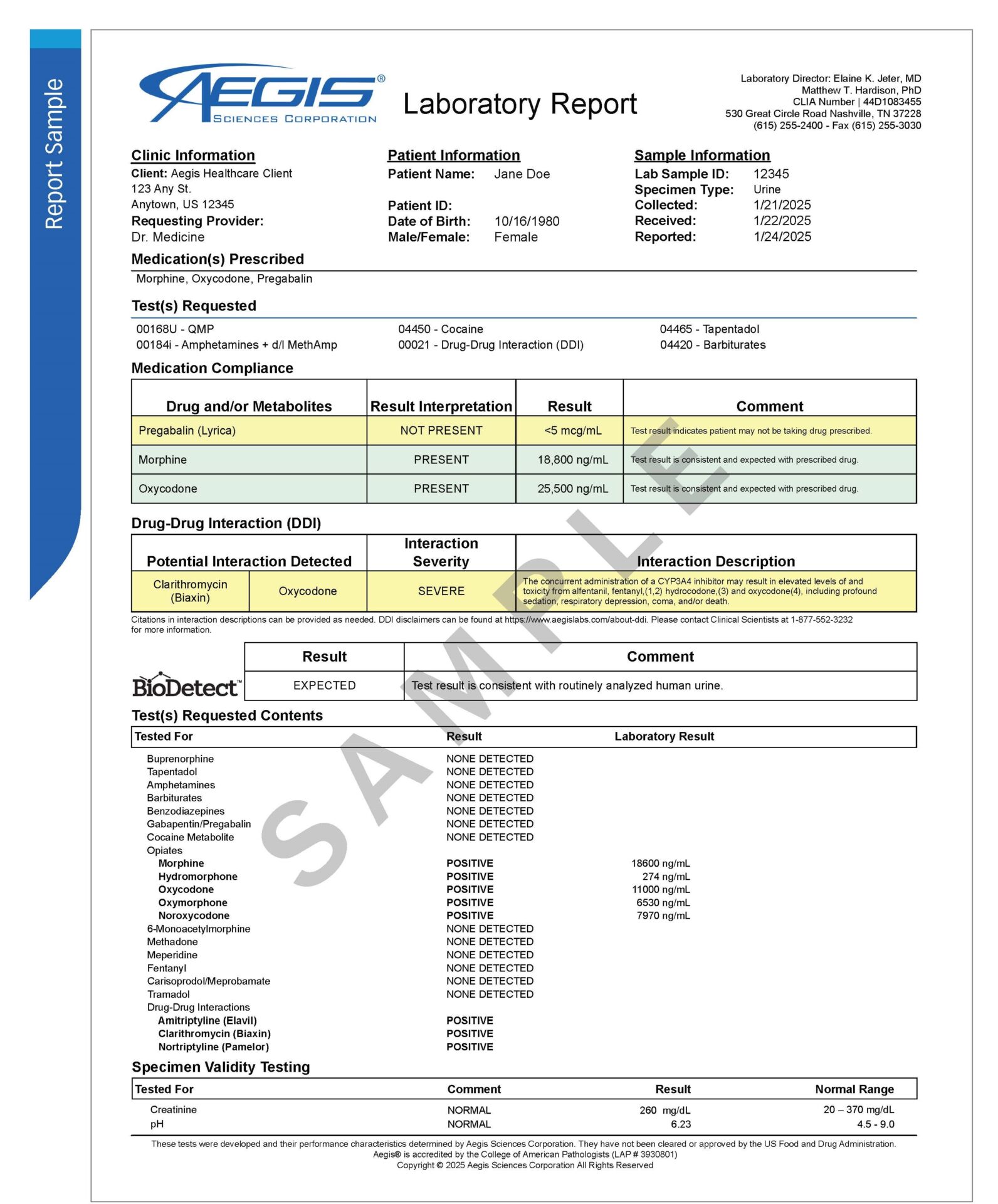
JD is a 39 year-old female who has been diagnosed with chronic lower back pain and fibromyalgia. During her scheduled visit with her pain management physician, she complains of feeling short of breath and expresses that she has fallen twice over the past two weeks. Based on her current medication regimen, the provider initially suspects newly developed intolerance to her prescribed dose or overuse of her medication reserved for breakthrough pain. The patient reports being compliant with prescribed medications and denies the use of any other medications.
The patient is currently prescribed:
• Morphine 15 mg ER every 12 hours for chronic pain
• Oxycodone 10 mg IR every 6 hours as needed for pain
• Pregabalin 150 mg twice daily for fibromyalgia
Solution
The pain management physician orders Aegis’s medication adherence testing and InterACT Rx™ tests to confirm adherence and further optimize the client’s therapeutic regimen.
Results of the definitive urine testing confirm the presence of oxycodone and morphine in the absence of pregabalin. InterACT Rx detected the presence of clarithromycin, a macrolide antibiotic and CYP3A4 inhibitor. The concurrent use of clarithromycin and oxycodone can result in a severe interaction risk for elevated levels of oycodone and increased risk of central nervous system (CNS) and respiratory depression.
The patient’s combination of prescribed medications provides both extended and immediate release options for the treatment of pain, as well as providing an option that is better suited for the treatment of fibromyalgia. Signs and symptoms of central nervous system depression could easily be interpreted as inappropriate use of her prescribed therapy.
Short-term medications, such as antibiotics, prescribed by a physician that is not involved in a patient’s routine care are often omitted from medication reconciliation. As is reported, clarithromycin can inhibit the metabolism of oxycodone and contribute to adverse effects associated with the drug. This can be particularly risky in patients that are concomitantly prescribed other CNS depressants.
Outcome
After discussing the results with the patient, the provider learned that the patient was recently diagnosed with pneumonia, and she received a course of clarithromycin to treat her respiratory infection. InterACT Rx gave this provider objective information about what the patient actually ingested allowing for a better understanding of what had contributed to this patient’s adverse effects. In this case, the provider was able to counsel the patient regarding risk of concurrent ingestion of clarithromycin and oxycodone and coordinate care with the physician treating the patient’s respiratory infection without significantly changing her pain management therapy.
These results can be used to drive conversations with patients, and improve therapeutic decision making.